Introduction: Evidence-based guidelines for patients with Multiple Myeloma (MM) acknowledge the importance of frailty status when deciding on treatment. Frailty status may also influence patient outcomes throughout cancer treatment. Electronic Patient Reported Outcomes (ePROs) effectively capture the real-world patient experience as it relates to frailty status and health outcomes. Using ePROs, this study explored symptom burden, symptom bother, physical function, and quality of life across fit, intermediate, and frail patients with MM.
Methods: All consenting adult patients with a MM diagnosis and current evidence of treatment were enrolled in the Carevive PROmPT® remote symptom monitoring platform between September 1, 2020 and March 10, 2023. Demographic and clinical characteristics were captured at baseline, including age, sex, race, frailty status, comorbidities, and social determinants of health. Classification of a patient's frailty status (fit, intermediate, or frail) involved triangulating data from three separate sources: Carevive's electronic Geriatric Assessment (eGA), the Cancer and Aging Resilience Evaluation (CARE) geriatric survey, and self-reported activity level. Validated psychometric tools were also used weekly to capture each outcome of interest, including symptoms (PRO-CTCAE), treatment bother (FACT-GP5), physical function (PROMIS-4a) and quality of life (EORTC QLQ #29-30). All results were stratified by frailty status.
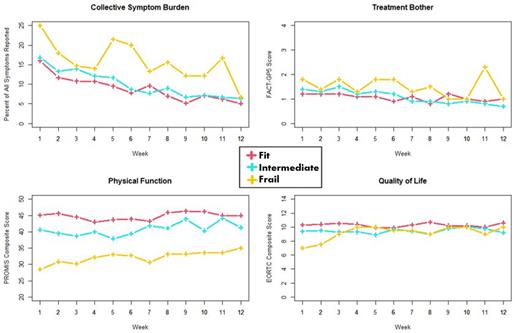
Results: A total of 151 patients were included in analysis. The median age was 66 (range 20-87), more than half were male (56%), the majority were white (75%), and most had at least one comorbidity (56%). The median follow time was 12 weeks (range 1-57). Frailty status was successfully classified for 147 (97%) patients and 99% of patients with 12+ weeks of follow up; among those classified, 93 (63%) were fit, 42 (29%) were intermediate, and 12 (8%) were frail. Across all patients, the most frequently reported symptoms were general pain (23% across all patient-weeks), numbness and tingling (23% across all patient-weeks), and fatigue (21% across all patient-weeks) (See Figure). Symptom burden was considerably lower for fit (16%) and intermediate (16%) patients at the start of their treatment compared to frail patients (25%). However, all patients had a consistent reduction in symptom burden over time (Fit - Week 1: 16%, Week 12: 5%; Intermediate - Week 1: 16%, Week 12: 6%; Frail - Week 1: 25%, Week 12: 6%). Physical function exhibited no change across 12 weeks. However, the non-static levels were consistently highest for fit patients, followed by intermediate patients, and then frail patients. On average, physical function was two-fold higher for fit patients compared to frail patients. Treatment bother and quality of life were comparable over time across all levels of frailty. However, on average, frail patients began treatment at a lower level of quality of life.
Conclusions: This study illustrates the feasibility of using remote symptom monitoring for gathering data on frailty status, symptom burden, treatment bother, physical function, and quality of life for patients with MM. Findings suggest there may be functional differences in the overall patient experience at different levels of frailty. This further supports the importance of using frailty status in oncology care, especially to identify actionable risk factors for poor health outcomes during cancer treatment.
Disclosures
Jamy:Ascentage: Other: Advisory Board Participation.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal